Prostatitis is the infection or inflammation of a man's prostate gland. Two million cases are diagnosed in the United States each year, with 5 to 9 percent of all men experiencing the condition during their lifetimes. Additionally, those who have had the condition before have an increased risk of recurrence.
While prostatitis can result from a bacterial infection, or occasionally an injury to tissues in the pelvic area, in most cases the cause is unknown. When bacterial related, infection can start when bacteria carried in urine leaks into the prostate.
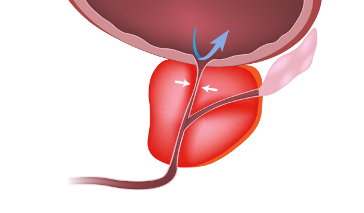
The Prostate Gland
The prostate—part muscle, part exocrine gland—sits below a man's urinary bladder and in front of his rectum. It wraps around the urethra (the tube that carries urine from the bladder out of the body) and produces a milky white fluid that is part of semen. It also helps propel semen during ejaculation.
Prostatitis Symptoms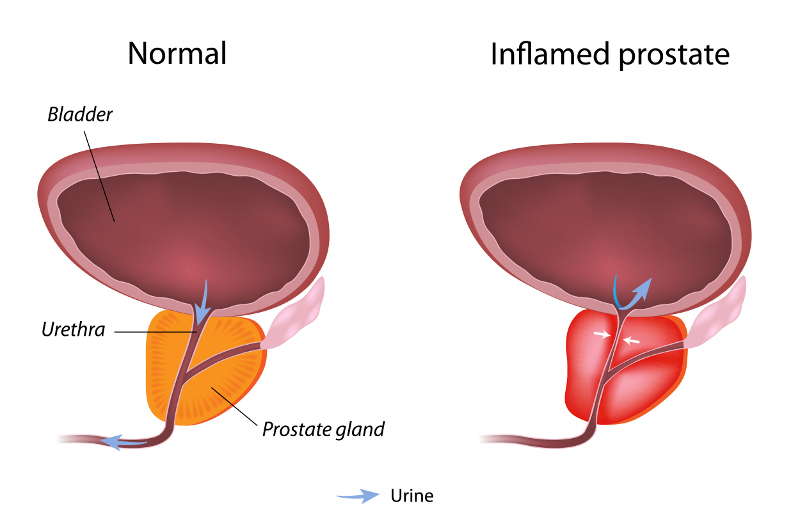
Symptoms can be similar to those of other conditions (such as bladder or urinary tract infections), and include:
- Painful, frequent, or difficult urination
- Fever
- Pain in the low back
- Pain in the testicles, penis, or perineum (the area between the testicles and the anus)
- Erectile dysfunction
- Decreased desire to have sex
- Painful ejaculation
Types of Prostatitis
Depending on symptoms and whether an infection is present, prostatitis can be categorized into four types:
- Chronic nonbacterial prostatitis and chronic pelvic pain syndrome (CPPS)
- Acute bacterial prostatitis
- Chronic bacterial prostatitis
- Prostatitis with no symptoms
Chronic nonbacterial prostatitis and chronic pelvic pain syndrome (CPPS)
This broad category of prostatitis is the most common, accounting for nearly 90 percent of all cases. The exact cause of inflammation is unknown (some studies indicate it may happen when tissues in the pelvic area are injured), but the inflammation itself can be identified if white blood cells are found in semen.
Acute and chronic bacterial infection
Acute and chronic bacterial prostatitis are caused by bacterial infections in the prostate. While acute prostatitis typically resolves with treatment, chronic prostatitis can return as often as every few months, even after treatment.
Escherichia coli, which originates in the intestines, is found in 65 to 80 percent of bacterial prostatitis cases. In one study, signs of another bacterium--a species of Corynebacterium--appeared in 65 percent of men with chronic prostatitis. Both E. coli and Corynebacteria can also cause other types of urinary tract infections, such as those associated with the bladder, kidney, and urethra.
Some sexually-transmitted diseases (STDs), such as chlamydia, can also lead to prostatitis. Most cases, however, are not STD-related.
Prostatitis Without Symptoms
Men can also have asymptomatic prostate inflammation. This type of prostatitis is typically discovered during routine exams for other conditions, such as infertility or elevated PSA (prostate-specific antigen) levels. The PSA test is sometimes done to assess a man's prostate cancer risk. But prostatitis can also be to blame for increased PSA and treating the condition often returns PSA to normal levels.
Diagnosis and Tests for Prostatitis
Because there are different kinds of prostatitis and the symptoms are not always clear, it can be a difficult condition to diagnose.
Certain tests indicate infection or inflammation in the urinary tract and prostate:
- Urine analysis is used to look for the presence of bacteria in the prostate; this is also done to rule out other kinds of urinary tract infections.
- Prostate secretions can be analyzed to look for the presence of white blood cells.
Prostatitis Treatment
Treatment of prostatitis depends on the cause and severity of symptoms.
References
Ferri FF. (2012). Prostatitis. Ferri’s Clinical Advisor 2013, 1st ed.
Nickel JC. (2011). Prostatitis and related conditions, orchitis, and epididymitis. Campbell-Walsh Urology, 10th. ed.
Murphy AB, Macejko A, Taylor A, Nadler RB. (2009). Chronic prostatitis: management strategies. Drugs. 69(1):71-84.
Chronic nonbacterial prostatitis and chronic pelvic pain syndrome: Current options for dealing with the most common form of prostatitis. (2007). Perspectives on prostate disease. Harvard Medical School. Vol. 1 No. 3
Stevermer JJ, Easley SK. (2000). Treatment of prostatitis. Am Fam Physician. 61(10):3015-3022.