da Vinci sacrocolpopexy is a minimally invasive procedure that uses a combination of laparoscopy and robotics to treat pelvic organ prolapse, a medical condition in which organs in a woman's pelvis—the vagina, uterus, rectum, bladder, urethra, and/or small bowel—move lower than their normal positions in the belly.
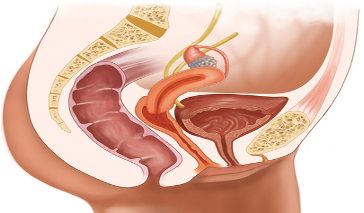
Pelvic organ prolapse occurs when the pelvic floor muscles that hold the organs in place become weakened or stretched due to childbirth, surgery (hysterectomy), excessive weight, pelvic organ tumors, frequent constipation, or a chronic cough. This can cause pelvic tissue or organs to extend to or outside of the vaginal opening. The condition can also lead to leakage of urine, problems urinating or passing stool, pressure in the pelvis, and sexual difficulties. While the condition doesn't present as a major health issue—it may get better or worse with time—da Vinci sacrocolpopexy is an option for treatment.
About da Vinci Sacrocolpopexy
Sacrocolpoplexy is a surgical technique that is used to treat two specific types of pelvic organ prolapse: vaginal and bladder. During surgery, the vagina is freed from the rectum and bladder so that a graft created from synthetic mesh can be used to cover both the front and back of the vagina. The mesh is then fastened to the large triangular bone located in the upper back of the pelvis (sacrum). By doing this, the vagina and bladder are lifted into their correct positions. A layer of tissue that lines the abdomen (peritoneum) covers the mesh, which keeps the bowel from attaching to it.
Traditionally, sacrocolpopexy has been done as an open surgery, whereby a large incision is made in the lower belly to allow the surgeon to access the pelvic organs. While the success rate for open surgery is high, there is more bleeding and it requires a longer recovery time—up to six days in the hospital.
Another option is laparoscopic sacrocolpopexy, in which surgical tools and a tube with a light source and camera at its tip (laparoscope) are inserted through several small incisions in the belly to perform the procedure.
da Vinci sacrocolpopexy is similar to laparoscopy, except it is done with a robotic surgical system. The surgeon controls the surgical tools and laparoscope—held by robotic arms—from a console rather than by handling them directly. Because the arms can bend and rotate further than the human wrist, more precision is attained.
Benefits of Da Vinci Sacrocolpopexy
The da Vinci system offers several benefits over open surgery:
- High-definition 3D camera with magnification
- Smaller, more precise movements of the surgical tools
- Insertion of tools through several small incisions
- Less pain and blood loss
- Less scarring
- Faster recovery and shorter hospital stay
- Fewer complications
Risks of da Vinci Sacrocolpopexy
Every surgery carries potential risks. For da Vinci sacrocolpopexy, these include:
- Infection
- Bleeding
- Injury to nearby organs
- Reaction to the anesthesia, mesh, or other implants
da Vinci Sacrocolpopexy Prognosis
Up to 90 percent of women who have sacrocolpopexy are relieved of their prolapse and associated symptoms. However, there is a risk that the prolapse can occur in a secondary part of the vagina, like the front wall that bears the bladder. Should this happen, further surgery may be required.
References:
Boyles SH, Weber AM, Meyn L. (2003). Procedures for pelvic organ prolapse in the United States, 1979-1997. Am J Obstet Gynecol 188(1):108-15.
Jelovsek JE, Maher C, Barber MD. (2007). Pelvic organ prolapse. Lancet 369(9566):1027-38.
Kramer BA, Whelan CM, Powell TM, et al. (2009). Robot-assisted laparoscopic sacrocolpopexy as management for pelvic organ prolapse. J Endourol 2:283-286.
Luber KM, Boero S, Choe JY. The demographics of pelvic floor disorders: current observations and future projections. (2001). Am J Obstet Gynecol 184(7):1496-501; discussion 1501-3.
Olsen AL, Smith VJ, Bergstrom JO, et al. (1997). Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501-6.