Relaxed vaginal outlet occurs when the tissues that separate the vagina from the rectum become weak or damaged, causing either the bladder, urethra, uterus, rectum, or small intestine to slip into or protrude from the vagina. This disorder often causes a variety of additional conditions.
When pelvic organs slip out of position, it can cause involuntary urine leakage, sudden urges to urinate, or fecal incontinence. Pelvic floor training, vaginal cones, biofeedback, electrical stimulation, and surgery can all help repair the damage.
Nonsurgical Treatment Options for Relaxed Vaginal Outlet
Before treating the condition, a urologist must first perform a physical exam to determine the extent of damage to the pelvic muscles, tendons, and ligaments. Based on those findings he can prescribe treatments, many of which are noninvasive or require only physical therapy and exercises that can be done at home.
Kegel Exercises
Kegels are a form of pelvic-floor muscle training that requires a woman to isolate and contract her pelvic floor muscles. Stopping and starting the flow of urine can help pinpoint which muscles these are. When doing Kegels—either lying or sitting—the bladder should be empty and the muscles should be contracted in sets of 10 (held for 10-20 seconds) while the butt, thighs, and abdomen are relaxed. In between each set of contractions, relax the muscles for 10 seconds. When done three to five times a day, or in five-minute sessions twice a day, symptoms can improve within six to 12 weeks.
Vaginal Cones
Some people have trouble performing Kegels because they cannot feel where the muscles are. Vaginal cones help women target and strengthen those muscles. Pelvic cones have a slight weight to them so that, when a woman sits upright, her pelvic floor muscles must remain contracted to keep the device in place. As muscle strength increases, cone weight can be increased. Pelvic floor muscle tone should improve after six weeks of regular exercise. After three months, urinary incontinence should lessen and even verge on going away entirely.
Biofeedback
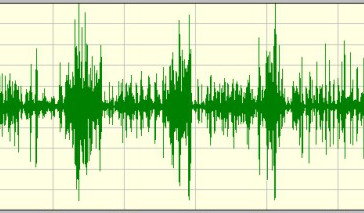
Biofeedback uses a variety of sensors to gain more information about how certain muscles—in this case, the pelvic floor—are functioning. During biofeedback training, a tiny sensor is placed either in or on the outside of the vagina, while additional sensors are placed on the buttocks or the abdomen. A computer connected to the sensors displays a graph of the pelvic floor muscle contractions on a screen so that the patient can see when she is tensing them properly. Electrical stimulation may also be used to encourage contractions and further strengthen the pelvic floor. Biofeedback therapy sessions are continued until the patient understands how to correctly contract her muscles, usually within three sessions.
Pessaries
Vaginal pessaries are removable devices that are placed into the vagina to help support the pelvic organs and decrease urinary incontinence. They come in a variety of different shapes and sizes, as well as materials. When combined with pelvic floor muscle strengthening, studies have found the levator hiatus is narrowed. Pessaries, alone, only relieve symptoms but do not strengthen pelvic floor muscles. It may take three to four months before results are seen, and long-term use may be needed for those with stress urinary incontinence and pelvic organ prolapse.
Surgical Options for Relaxed Vaginal Outlet
Surgical procedures aim to reinforce the area of weakness by either suturing it or adding synthetic or biological support in the form of graft materials. Surgery is reserved for those cases in which nonsurgical treatment methods have failed, for when relaxed vaginal outlet is coupled with rectocele (front wall of the rectum bulges into the back wall of the vagina), or for when the condition is symptomatic and severe. Patients require about 4 to 6 weeks to completely heal, and complications can include transient urinary retention (12.5 percent), vaginal erosion (13 percent), or extrusion (8 percent).
Prognosis for Relaxed Vaginal Outlet
Pelvic floor strengthening can improve relaxed vaginal outlet symptoms and its additional conditions, and is effective anywhere between 50 to 80 percent of the time. Surgical treatments have an even higher cure rate—between 80 and 95 percent for patients with traditional and site-specific rectocele—but surgery carries a far higher risk of infection and pain.
References
Abet E, Lehur P, Wong M, et al. (2012). Sexual function and laparoscopic ventral rectopexy for complex rectocoele. Colorectal Disease; 14(10):e721-e726.
Cespedes, RD. (2011). The treatment of posterior compartment vaginal defects. Urologic Clinics of North America; 38(1): 17-23.
Barber MD et al. (2009) Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 114(3):600-9.
Weber AM, Walters MD, & Piedmont MR. (2000). Sexual function and vaginal anatomy in women before and after surgery for pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol; 1610-1615.
Mattingly RF, & Thompson JD, eds. (1992). Relaxed vaginal outlet, rectocele, fecal incontinence, and rectovaginal fistula. TeLindes Operative Gynecology. 7th ed. Philadelphia, Pa: JB Lippencott.